Surgical Correction for Chest Deformity (Funnel Chest; Pectus Excavatum and Pigeon Chest; Pectus Carinatum)
Hiroshi Iida MD, PhD, Chief Surgeon, Division of Chest Wall Surgery
Funnel chest (pectus excavatum) is the most common congenital chest deformity, occurring in approximately 0.1% of births. About half of patients have family history of chest deformity. A study in United States revealed that chest deformity did not have effects on life span. We have been developing surgical procedure for chest deformities since 1984.
We introduce our methods of pectus excavatum repair in which the introduction of exogenous material is not a requirement. Our method is able to adapt for pectus carinatum (pigeon chest) too without difficulties.
Symptoms and Clinical Examinations of Chest Wall Deformities
Patients of pectus excavatum sometimes complain physical symptoms such as dyspnea on effort, diminished endurance, palpitation and chest pain, as well as cosmetic or psychological impairment. Adult patients tend to have more complaints than pediatric patients, and about 60% of adult patients have physical complaints. Patients are sometimes pointed out abnormalities on clinical examinations including ECG change, enlargement of heart shadow in chest X-ray, borderline respiratory function test, and abnormal sign in ultra-sound cardiogram. These do not indicate inferior functions of the heart and lung. Because the patient’s heart is pushed by chest wall and change position, clinical examinations dates may change. Most of symptoms and physiological data improve after surgery. Patients with pigeon chest usually do not have physical complaints, however, protrusion on their chest may be obvious through their clothes on, and brings them psychological inferiorities.
About our Patients
From July 1993 to 2020, 608 patients underwent repair of chest deformity. Mean age was 16.2, ranging from 3 to 56 years of age. The indication for surgery was decided by a visual comparison of the depth and volume of the excavation with the patient's clenched fist. If the depth and volume of the excavation were observed to exceed that of patient's fist, the patient was recommended for surgical repair.
Operative Technique
Sterno-costal elevation modification 3 (SCE3) is our standard method.
Sterno-Costal Elevation Modification 3 (SCE3)
A median vertical incision was made superficial to the defect, in female patients an inframammary incision with upward curvature in the middle was sometimes used to reduce scar visibility. A part of the third or fourth to the seventh costal cartilages was resected. The lower part of the sternum below sixth cartilage junction was also resected. This part of the sternum tilts back toward the vertebrae and exerts pressure on the heart. All of the stumps of cartilages were pulled and reattached to the sternum using surgical sutures (Fig. 1). The number and length of cartilages resected was determined by the degree of deformity. In the case of asymmetric deformity, different lengths and different numbers of cartilages were resected on each side. The secured ribs pulled the sternum toward both sides, such that the resultant force caused the sternum to raise anteriorly, while protruding costal arches, which were frequently observed in patients with funnel chest, and irregularities of the chest wall was pulled and corrected by counter action (Fig. 2). Since all of the cartilage stumps were secured, the tension exerted by the patient's ribs was enough to flatten and fix the sternum without exogenous materials and cortical osteotomy of upper sternum, but did not disturb respiration. Some further modifications may be used to correct sever asymmetry. The muscles were secured to the position where they were. The repair was completed by one-time procedure without leaving exogenous materials except suture. Recommended age for surgery is under 20 yo. Chest wall of patients in this age has malleability. Most suitable age for SCE3 is 5 to 10 yo. We believe that it is important to relieve structural compression of the chest and allow normal growth of the thorax, and surgical repair can reduce potential physical and psychological impact. Children in this age range are sufficiently emotionally mature and are more likely to expect a positive experience from their hospital stay. Children at this age are also generally young enough not to have suffered psychological impairment secondary to the perception of abnormal body image. Our procedure does not keep patients waiting until after growth spurt of puberty. After age of 30, rib cartilages get calcification and become rigid and brittle. However, we do not exclude these patients from surgical candidate for chest wall correction. Because they frequently have severe physical complaints.
SCE3 can be adapted for pigeon chest. Protruded chest wall is corrected well by partial resection and re-fixation of rib cartilages.

Fig. 1
Surgical technique of sterno-costal elevation (SCE3). An area of the fourth to seventh costal cartilages was resected. (marked in blue). The lower part of sternum below sixth cartilage junction was also resected. All of the cartilage stumps were then affixed to the sternum with braided polyester sutures.
Results of the surgery
Mechanical ventilation was not needed after emergence from anesthesia, and all patients were returned immediately from the operating room to an ordinary ward, and none of them needed blood transfusion. The depression of the anterior chest wall was corrected (Fig.2-4), asymmetric chest walls reshaped to symmetric (Fig. 3), protruding costal arches were corrected (Fig. 4), and cardiac shadows observed in chest X-ray returned to near midline (Fig. 5). Chest deformity was remarkably improved in all patients. None of the patients have had fair or poor results. Post operative chest appearance of pediatric patients tend to be better than that of adult patients. The wound was inconspicuous, and most of the patients reported satisfaction with the wound and the shape of the corrected chest. The length of incision was 3.3+/-0.5 cm in patients under seven years old, and 3.5+/-0.5 cm in patients 7 to 11 years old, 5.0+/-1.1 cm in those aged 12 to 15, and 5.8+/-1.2 cm in over 16 years old.
None of the patients developed pneumonia, deep wound infection or any life-threatening postoperative complications. No reoperations were required in any of the patients for any reasons. Epidural analgesia was not needed in pediatric patients. Orally-administered analgesia was usually provided for up to 7 postoperative days in adult patients. In pediatric patients, analgesia was needed for only 2-3 days following surgery. None of the patients experienced residual pain.
Patients were able to return to their preoperative daily activities within a week of surgery. Our patients need not to use protective or corrective brace. Our patients went back to school or job one month after surgery. We advise our patients to avoid contact sports for three months as a precaution. They do not need to undergo any subsequent surgery. No patient has experienced severe deterioration of chest contour in follow up period even in pediatric patients.
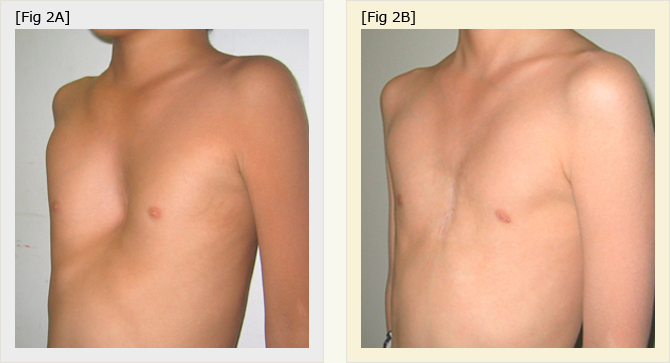
Fig.2A
Chest of 5 year-old boy with pectus excavatum before surgery.
Fig. 2B
Six month after sterno-costal elevation (SCE). The length of the wound was 3.5 cm. Normal chest contour was seen.
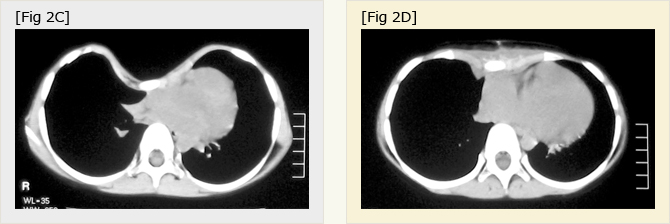
Fig.2C, D
Chest CT scan of the patient fig. 3 before (C) and after (D) SCE.
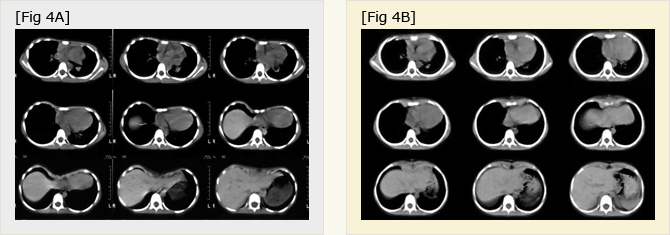
Fig.3AB
Chest CT scan of 4 year-old boy before (A) and after (B) SCE. Asymmetric chest walls reshaped to symmetric.
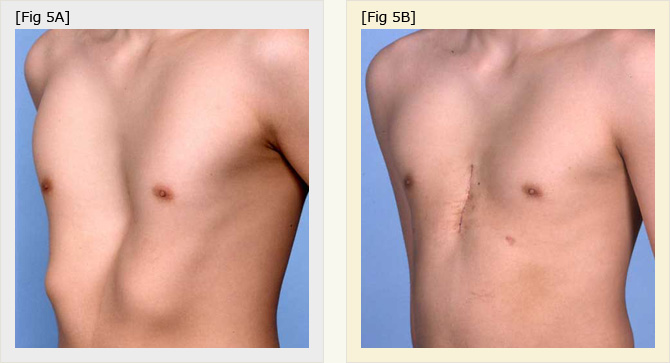
Fig.4A
Chest of 16 year-old male. Protruding costal arches were seen.
Fig.4B
Two weeks after SEC. Protruding costal arches were corrected.
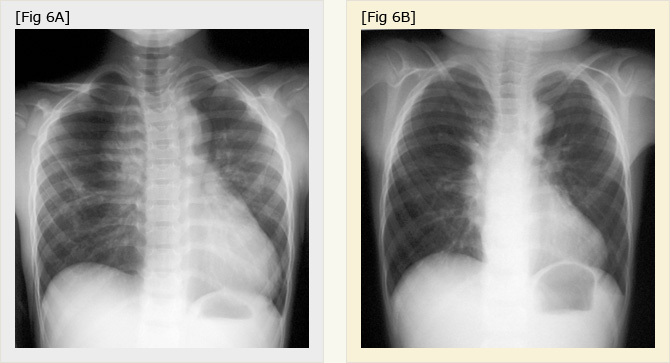
Fig.5
Chest X-ray of the patient of Fig. 2, before (A) and after (B) SCE. Cardiac shadow returned to near midline and scoliosis was improved.
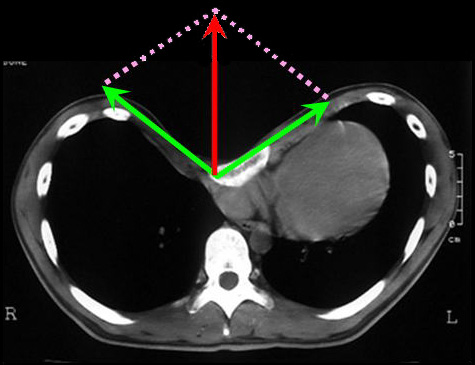
Fig.6
The sternum is pulled laterally by shortened and resutured costal cartilages (green vector), and the resultant force raises the sternum ventrally (red vector).
Other methods of funnel chest correction
After Myer et al. reported the correction for pectus excavatum in 1911, various methods have been reported. Most conventional techniques were based on methods described by Ravitch, including a long incision in the anterior chest wall, resection of deformed rib cartilages and the tearing of the upper sternal cortex. Wada et al described sternal turnover for pectus excavatum in 1970. We have developed this technique to make it less invasive. SCE3 does not include sternal turnover and tear of upper sternum.
A revolutionary procedure first reported by Nuss in 1998 has been described as minimally invasive repair for pediatric patients, because this approach does not require either an anterior wound or the cut of cartilage or sternum. In this procedure, a metal bar is placed behind the sternum through pleural spaces, and is secured to the ribs. The Nuss procedure has gained substantial popularity, but has also involved a relatively high morbidity rate. Perioperative and late complications including migration or infection of the bar, pneumonia, pleural effusion, hemothorax, wound seroma, skin necrosis, pericarditis and even cardiac perforation have been reported. Severe pain is one of the unpleasant complications of Nuss procedure. Some patients suffered from residual pain and required analgesia for extended periods. The bar(s) have to be left in the chest wall for years, and heavy contact sports are prohibited. Nuss did not recommend his method for patients before growth spurt in adolescence, because of high incidence of recurrence and complications. The metal bar is essential for Nuss procedure, and bar seems to be a main cause of complications. The chest wall moves with respiration and body movements, and grows for years, and the ribs are sensitive to the stress of being subjected to stabilization with a metal bar. In addition, the extent of the physical and mental burden that may be associated with the introduction of a foreign body into the chest of a growing, pre-adult patient remains unknown. Because the majority of pectus excavatum corrections are performed in young patients, and candidate for surgical correction are able to maintain acceptable quality of life preoperatively, surgeons have a strong obligation to avoid the risk of complications requiring long-term medical treatment or reoperation.
Summary
An excellent postoperative chest contour was achieved, and none of our patients developed major complications requiring long-term hospitalization or restriction of normal life. We believe that the risk of complications is one of the most important factors in determining the appropriateness of major surgical invasion, especially in pediatric patients. The procedures described here include the resection of cartilage, but we believe that our technique represents a less invasive and lower risk procedure for the repair of pectus excavatum for wide age range of patients.
About Shonan Kamakura General Hospital
Shonan Kamakura General Hospital is located 50km south from Tokyo. All of the hospital costs and surgical cost for the operation of funnel chest are covered with Japanese health care insurance for Japanese residents.
We are also open for foreigners. We have been accredited by Joint Commission International.
If there are further questions, please feel free to ask us. (funnel@shonankamakura.or.jp)
General Consultation Service Hours
【Morning hours】
12:30~ * Hours vary by department
【Afternoon hours】
12:30 ~ * Hours vary by department
※Some departments are by appointment only. Consultation Service Hours may vary by department. Please ask the clerk at the reception desk or call +81-467-46-1717 for further details regarding operating hours.
Days Closed
Sundays and Holidays
Shonan ER
Open 24 hours a day 365 days a year
※For more information, please contact us at +81-467-46-1717 or Fax +81-467-45-0190 or contact us.